Is inequality shortening your life span?
30th September 2013 · 0 Comments
By Phillip Longman
Contributing Writer
Editor’s Note: — This the final installment of the Kellogg Foundation-sponsored 11-part Series on Race in America — Past and Present – is a compilation of three articles joined together on the topics of health, health care and life spans of Americans and how they intersect with race and class.
(TriceEdneyWire.com) — Imagine you got to choose whether to be born Black or born white in America. Here are a few health statistics that might inform your decision:
If you chose to be born white, your chances of dying of Parkinson’s disease would be twice as likely as if you chose to be Black. Your chances of dying from cirrhosis of the liver or Alzheimer’s disease would be 25 percent higher. As a white person, you’d also be two and a half times more likely to commit suicide.
 Based on those facts alone, the decision to be born white might sound like a pretty bad idea. And sure enough, life doesn’t work out well for many millions of white people in America. But you might also consider that everyone has to die of something, and dying from these particular causes has some advantages.
Based on those facts alone, the decision to be born white might sound like a pretty bad idea. And sure enough, life doesn’t work out well for many millions of white people in America. But you might also consider that everyone has to die of something, and dying from these particular causes has some advantages.
As terrible as Alzheimer’s and Parkinson’s are, for example, almost no one dies of them unless they’ve previously managed to escape death from other causes for 75 years or more. Cirrhosis of the liver tends to kill at younger ages, but you can still spend many decades of hard drinking before it catches up with you. Even for the chance to commit suicide, one typically has to have survived at least until one’s teens, and suicide is more common among those who have succeeded in growing old than it is among those who are still young.
By contrast, consider the pros and cons of choosing to be born Black, based on life tables alone. To be sure, opting to be Black would reduce your chances of dying from diseases caused by risk factors that rise with age. But it would also severely reduce your chances of living to even your first birthday, let alone growing old enough to retire.
This would be particularly true if you chose to be Black and male.
To start with, your chances of dying before your first birthday would be roughly 2.3 times greater than if you were born white. If you managed to make it to age one as a Black male child, your chances of dying before your fifth birthday would be 80 percent greater. If you survived to age 15, you’d have a 60 percent greater chance of dying within the next 10 years. If despite these elevated risks of premature death you nonetheless managed to get to your 45th birthday, you’d still be 80 percent less likely to live long enough to collect Social Security than if you had chosen to be white.
If you were Black you would also, of course, substantially elevate your chances of growing up in a poor, crime-ridden neighborhood, and the health consequences of living in that kind of environment are extremely adverse. If your neighborhood were, say, New York’s Harlem during the 1990s, as a young man you’d have only a 37 percent chance of living to see 65. By contrast, according to a seminal study published in the New England Journal of Medicine, if you’d chosen to be white and wound up living in the unremarkable, predominantly white middle-class Detroit suburb of Sterling Heights, your chances of still being alive at 65 would be above 89 percent.
So what would you choose? It may be that longevity is not the only measure of the good life. You might also, with enough luck and fortitude, be able to overcome the highly elevated health risks of choosing to be born Black. Indeed, it is a curious fact that among African-American males who live to an advanced old age (85 years or older), the chances of living for another year are actually greater than for white males of the same age-presumably because the few African-American men who have survived that long have remarkable constitutions.
Yet who would ever choose to face this pattern of competing health risks across their life course? It’s far more important to have a good chance to become elderly in the first place than to embrace the tiny chance of becoming a centenarian in the unlikely event you’re not already dead by 65.
The vast disparities in health and longevity that exist between the races in the United States violate a fundamental idea of justice that we all carry with us at least to some degree. It is the idea of justice as fairness, of what kind of world we would choose to live in if, as the philosopher John Rawls framed it, we were all impartially situated as equals before being born and did not know what our station in this life would be. A society that resists ending the preventable causes of these racial disparities in heath is a society resisting justice.
But what are those preventable causes, and what could or should be done about them? To answer that question, let’s consider another thought experiment.
Imagine if, before you were born, you were told that you could choose to be born either Black or white in America. But if you chose to be white you would live in poverty and if you chose to be Black you would be in the lower-middle class. In this thought experiment, you wouldn’t know anything about what our world is actually like except for estimates of life expectancy for different categories of people.
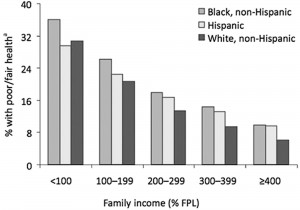
Those estimates would tell you that choosing to be white would bring you very little, if any, advantage to health if you were also poor. For example, according to data developed by the Robert Wood Johnson Foundation, approximately 35 percent of whites living below the poverty line report themselves to be in only poor or fair health. This is quite close, after we adjust for age differences, to the 32 percent of poor Blacks who report fair or poor health.
Meanwhile, the health status of Both Blacks and whites improves dramatically with higher income while the gap between them remains small. Among Blacks and whites living at just four times the poverty rate, for example, the percent who report poor or fair health drops to eight percent and six percent respectively. Your race per se, in other words, plays little role in predicting your health compared to your income.
What explains the residual difference in the health status of Blacks and whites who have the same-size pay check? Researchers suggest it may reflect in part the reality that at any given income level, Blacks tend to have fewer assets than whites, such as home equity and financial savings. A Black family earning, for example, $50,000 in income is less likely to own its own home, less likely to have received an inheritance, and more likely to be encumbered by debt than is a white family with the same income. Middle-class Black families are also more likely than middle-class white families to bear the health consequences of having lived in poverty in the past.
The gap in health status may also reflect the fact that among families with similar levels of income, as well as educational attainment, Blacks are more likely than whites to live in neighborhoods with higher concentrations of crime, poverty, pollution, liquor stores, “junk food” outlets, and inferior health care. Conscious or unconscious bias among healthcare providers may also be at work in explaining the racial health gap, though your chances of receiving substandard health care in the United States vary far more according to where you live than according to the color of your skin.
Yet even if they remain remarkably small at any given level of income, racial disparities in health do exist. And these disparities are large enough to make it rational (if health and life expectancy are the only criteria) to prefer being born a poor white American than a poor Black one. But the differences are also far too small to make it rational to prefer being born a poor white to being born a rich, or even lower-middle-class, Black. Again, the health status of Blacks who live at just above the poverty line is substantially better than that of whites who live below it.
There is a reason why, in English, we use the word “poor” to refer to both a lack of money and a lack of health. Both historically and still largely today, poor people are likely to have poor health, almost regardless of other circumstances.
That poverty is deadly is not hard to understand, at least at the extreme. To be very poor means not having enough to eat, being exposed to the elements, and living in areas where homicide and addiction are leading causes of death or where your access to appropriate health care is minimal or nonexistent. In addition, both historically and today, getting seriously sick is likely to make you seriously poor even if you weren’t before.
But if our goal is to overcome the vast disparities in health that exist in the United States, especially for African Americans, we have to absorb two more difficult facts. These facts are noncontroversial among epidemiologists, even if they remain unfamiliar to most Americans.
First, it’s not just extreme poverty that is bad for your health; so is having less autonomy and status than others, regardless of your income. Among people who have plenty to eat, have equal access to quality health care, live in safe neighborhoods, and hold down jobs, health and life expectancy declines with socioeconomic position. While it is not hard to understand why truly impoverished people of all races die younger than middle-class people, it’s also true that middle-class people die younger than upper-middle-class people, and that upper-middle-class people die younger than rich people, even though none but the very poor are wanting for the basic necessities of life.
The second fact is just as strange, and equally radical in its implications, both for individuals seeking to maximize their personal health and for societies that are intent on creating just institutions. It is that the wider the disparities in status and power that exist between people within a given workplace, city, county, state, or country, the more premature deaths happen. Crudely put, inequality kills.
It’s a pattern that’s found, in greater or lesser degree, under all forms of government, within rich countries and not-so-rich countries, in the East and in the West. It also holds true in countries with universal health care and those without, and among different U.S. states.
The first place researchers rigorously documented this pattern was in the United Kingdom. There, starting in the 1960s, a team headed by the epidemiologist Michael Marmot began a long-term study of the health of British civil servants. These bureaucrats had much in common with one another. None lived in poverty; none were rich. None had jobs that posed any clear physical danger beyond the risk of paper cuts. All had equal access to the fully “socialized” British health care system.
Yet as the study went on it became clear that these bureaucrats were vastly different from one another in their health and longevity. Specifically, among employees of the same age, those who occupied the bottom of the organization chart as typists, clerks, and the like were four times more likely to die over the next 20 years as were administrators at the top of the hierarchy. Moreover, the differences in death rates did not just exist at the extremes of the organizational ladder. At every step in between, health and life expectancy were better one rung above and worse one rung below.
At first, researchers suspected that this social gradient of disease must be related to lifestyle. People at the bottom of the organization tended to smoke more, for example. But it turned out that if you were an administrator and smoked two packs of day, this was far less dangerous to your health than if you were a clerk who did the same. Similarly, if your blood pressure or cholesterol levels were high, or if you rarely exercised, being higher in the organizational chart made these conditions less threatening to your health than if you were lower. This was true even though people at the bottom of the organization tended to see doctors more frequently.
Since then, similar correlations between health and social rank have been observed just about everywhere researchers have looked. To take just one of the more curious examples, it turns out that Hollywood actors who win the Academy Award live four years longer on average than their costars in the same movie. And they also live four years longer than actors who were nominated for the award but did not win. This four-year difference in life expectancy may not sound like a lot. But to keep the implications for population health in perspective, consider that if all deaths from heart disease were magically eliminated while deaths from other causes remained the same, the improvement in life expectancy for the population as a whole would come to just four years.
One way researchers have tried to explain these and similar findings is to posit that the losers in our society have become losers because they have poor health. This is no doubt true in some cases. Clearly, if you’re in the hospital for months following a car crash, lose the ability to walk, and go through life thereafter with hideous facial scars, it is bound to negatively affect your career prospects. The same would be true if you were born already addicted to narcotics or positive for HIV.
Or to take a less extreme but far more common example, say you are a low-level employee working a dead-end cubicle job and find yourself afflicted at age 30 with prolonged bouts of depression, insomnia, and more than an occasional hangover. It is possible that these conditions will make it less likely that you will rise to the top of the ladder than if you bounced out of bed each morning feeling like the picture of health.
But to conclude in this instance that your lack of upward mobility is because of your poor health is to beg the question of why you have developed these afflictions in the first place. Maybe you would drink in any event. Maybe you’d describe life as stressful regardless. But would you drink as much, and feel so bad about it in the morning, if you also felt (like that famous, highly effective, long-lived alcoholic Winston Churchill) that you were in command and getting important stuff done?
To continue this thought experiment, what if you did not feel slighted and powerless at work; if your boss didn’t make eight times your income but only double; if he didn’t seem to look down on you and “your kind”; if losing your job didn’t mean losing what little control you have over your life? What if you didn’t feel variously envious, intimidated, and infuriated by coworkers, neighbors, and people you see on TV who seem to have it all; if you could point to some way of keeping score in this life by which you were a winner and life had meaning?
The specific biological mechanisms that lead from feelings of relative powerlessness and low status to specific diseases are not well understood at the molecular level. Some researchers have pointed to the role of cortisol, a steroid hormone released by the adrenal gland in response to stress that has the effect of suppressing the immune system. Among people who are overweight, those with high levels of cortisol are more likely to contract diabetes than those with low levels.
More than 200 laboratory studies have also shown that the highest cortisol levels are found in people required to perform tasks outside their control that involve, as the epidemiologist Richard Wilkinson puts it, “threats to self esteem and social status in which others can negatively judge your performance.” A hard-charging executive may use the word “stress” to describe his reaction to the burdens of command, but it is his cowering subordinates who are most likely to feel the kind of stress that literally changes body chemistry.
The negative effects may be compounded if those subordinates must also endure the stress and humiliation of either perceived or real racial or class discrimination. And the effects may be further multiplied if they have also internalized feelings of inferiority based on these or other negative stereotypes or social constructions.
In an intriguing study at Emory University, researchers found, for example, that Black men who reported being victims of racial discrimination experienced an increased risk of heart disease. But a much greater risk of heart disease was found among African-American men who agreed with negative statements about Blacks. Indeed, the highest rates of heart disease were found among African-American men who said they were not personally victims of racial discrimination but still viewed their own race as inferior. Put another way, being or believing yourself to be the victim of racial discrimination is not good for your health, but what’s really bad is to absorb a social belief system that says you are at the bottom.
Cross-country comparisons also establish a clear link between poor health and social stratification. Among developed countries, for example, there is no correlation whatsoever between per capita GDP and life expectancy. But there is a strong correlation between countries that have low levels of inequality and those in which long lives are most common.
Sweden and Japan, for example, are very different countries, but both have extremely low levels of income inequality and the lowest rates of premature death in the developed world. Sweden achieves its egalitarianism through a large welfare state that massively redistributes income and opportunity. Japan has a comparatively small welfare state, but, according to custom, bosses refrain from paying themselves too many multiples of what workers earn. For the purposes of maximizing public health, Wilkinson observes, it does not seem to matter how a nation achieves relative equality, only that social and economic stratification is somehow kept to a minimum.
A similar pattern emerges when we compare how long white people live in different parts of the United States. To better see what happens, consider one last thought experiment.
Suppose, before you were born, you were told that you had to be a white man, but you could choose whether you would live out your days in Mississippi or Minnesota. If you could not know anything else about these states except their life tables, what would the rational choice be?
The life tables would tell you that if you wound up a white man in Mississippi, your chances of not dying before age 65 would be little better than 74 percent, and that if you did live to that age, you could expect to be dead within 15.35 years. But if you were a white man in Minnesota, your chances of living to age 65 would be better than 83 percent and your remaining life expectancy at that point would be 17.49 years.
The choice would seem clear, but what explains how stark it is? One big difference between Mississippi and Minnesota is the number of Black people in each state. But unless you think that Blacks in Mississippi are responsible for the deaths of huge numbers of white males-and they aren’t-that can’t be the reason why white men in Mississippi live shorter lives than white men in Minnesota. Nor are differences in median household income between whites in Mississippi and Minnesota large enough to explain such a large disparity in health: few whites in either state are poor enough that their health is threatened by lack of food or shelter.
The key factor may be how these states differ in their degree of social and economic stratification. Mississippi is among the states with the highest inequality of income. Moreover, throughout most of the last two decades Mississippi has led the nation in the growth of income inequality, whether as measured by the difference between those at the very top and those at the very bottom or by the gap in income between the middle class and the very rich.
Minnesota, by contrast, has much lower disparities of income, and is much more egalitarian in many other dimensions as well, including educational attainment, access to health care, and even, dare we say, cultural style. Garrison Keillor’s joke about all the kids in Lake Wobegon being “above average” contains an important truth: Minnesota is not a place where invidious distinction is typical, or kindly looked upon. And perhaps because of that, it is also not a place where stress and insecurity about social standing and loss of face is very common.
Within the United States generally, disparities in health among different segments of the population have increased in lockstep with growing disparities in income and education. By now it’s to the point that poorly educated white Americans, for the first time ever, are experiencing an absolute decline in their average life span. white males with fewer than 12 years of education now have a life expectancy of just 67.5 years-just six months longer than the standard Social Security retirement age set under current law for today’s middle-aged and younger Americans. The gap in life expectancy between white females who go to college and those who don’t widened from 1.9 years in 1990 to 10.4 years in 2008.
Meanwhile, for all but those at the very top of the ladder, and perhaps even for them, life is shorter than it likely would be if we lived in a more equal, less socially competitive and status-driven society-including one that was less obsessed with status distinctions based on race, education, and profession or that paid less notice than Americans have since the 1980s to who has the biggest McMansion, the most designer clothes, or the latest, snazziest smartphone. Inequality may not be an equal-opportunity killer, but few escape its mortal consequences.
To Live Longer, Move to a New Zip Code
Michelle Obama’s “Let’s Move” campaign emphasizes the importance of physical activity for combating obesity, a point she has driven home by dancing alongside school kids to Beyoncé’s workout video. But another kind of movement may also be important to your chances of living to a ripe old age: moving to a new zip code.
Between 1994 and 1998, the U.S. Department of Housing and Urban Development conducted a demonstration project known as “Moving to Opportunity.” The project randomly assigned low-income families to one of three groups. Those in the first group received a voucher that they could use to help pay the rent on an apartment, provided that the apartment was not in a low-income neighborhood. Those in the second group received a voucher they could use in any neighborhood, while those in a control group received no voucher.
In 2011, HUD researchers published the results in the New England Journal of Medicine. The most dramatic finding was that people assigned to the different groups varied significantly in their weight by the end of the experiment. Going into the program, participants as a whole had been substantially more obese than the U.S. population as a whole. But 10 to 15 years later, those women who had moved to more affluent neighborhoods were one-fifth less likely to be obese than those in the control group, and also one-fifth less likely to have contracted diabetes.
This was true even though there was little difference among all the participants in the numbers who managed to move off welfare, improve their education, or find a better job. This suggests to researchers how powerfully our surroundings alone are to determining our habits and health. Though it might seem strange to say that obesity is contagious, for example, it does seem that people’s risk of it is affected by the weight of their neighbors, as well as by such environmental factors as whether most of the food for sale in their environs is junk food, as is often the case in America’s most impoverished neighborhoods.
The results of the HUD demonstration project are in line with other studies showing the extreme importance of geography and social environment as determinants of health. A dramatic graphical representation of this reality can be seen in the accompanying map of the Washington, D.C., metropolitan area developed by the Commission to Build a Healthier America. It shows how life expectancy improves by nearly a decade within just a few stops along the region’s various Metro subway lines.
Color-Blind Medicine?
In 2002, the Institute of Medicine published an oft-cited and controversial report entitled “Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care.” The report concluded that members of minority groups, even when fully insured, tend to receive substandard care from their doctors. It cited disparities in how often whites and minorities received even routine medical procedures, as well as how often they underwent specific operations, such as coronary artery bypass surgery.
The resulting headlines were sensational-“Is Your Doctor a Bigot?” asked one. And there soon followed fulsome denunciations of the report’s conclusions, notably by Dr. Sally Satel and Jonathan Klick of the American Enterprise Institute. In their 2006 book, The Health Disparities Myth, Klick and Satel claimed that “[n]ot only is the charge of bias divisive, it siphons energy and resources from endeavors targeting system factors that are more relevant to improving minority health.”
Today, both sides in this debate have refined their positions and can point to new information. Professor David R. Williams of the Harvard School of Public Health still criticizes Satel as “coming at it from an ideological perspective.” But, he adds, “I will say one thing in her defense. At the time of the IOM report, our conclusion about the role of unconscious discrimination was based on circumstantial evidence.”
That changed in 2007, when the Journal of General Internal Medicine published the results of a study of residents at four academic medical centers. Participants were asked to review the medical record of an imaginary patient complaining of chest pain. For half the participants, the record included a picture of a middle-aged Black man; for the rest, a middle-aged white man. Participants were asked to rate on a scale of 1 to 5 whether they thought the patient suffered from coronary artery disease, and, if so, whether they believed that the patient should receive a drug treatment known as thrombolysis.
The study also asked participants to complete what are known as Implicit Association Tests, or IATs. These tests are designed to uncover unconscious bias by, for example, asking test takers a series of questions about whether they associate the word “happiness” with the word “white” or with the word “Black.” In this instance, the test also asked the residents whether they associated Black patients with being more or less cooperative with a doctor’s orders.
The study found that participants who scored high for anti-black bias on the IATs were less likely to recommend thrombolysis when the Black man’s picture, rather than the white man’s, was included in the medical record, presumably because they believed the Black man would be a less cooperative patient or perhaps less able to pay. The study’s authors concluded that the “[r]esults suggest that physicians’ unconscious biases may contribute to racial/ethnic disparities in use of medical procedures such as thrombolysis.”
While few now dispute that some doctors may consciously or unconsciously treat patients of color differently, both the nature of that bias and its importance in explaining racial disparities in health care are highly disputed. For example, in focus groups organized by researchers to assess the role of race in medical practice, Black doctors were far more likely than white doctors to say that a patient’s race is a medically relevant factor in determining the best treatment.
As one Black physician in a Philadelphia focus group put it, “I think being an African-American is a risk factor in and of itself. And, I think that when you see an African-American then you need to often be more aggressive than you would, and use different standards than you would for the general white population.”
Black doctors were also more likely than white doctors to say that they pay close attention to whether a patient can afford the prescriptions they write, and to consider what the circumstances of their patients’ lives are like outside the examining room. In contrast, white doctors in these focus groups tended to dispute that there is any reason to pay attention to a patient’s race in recommending a course of treatment, and even to warn other doctors against racial stereotyping.
But perhaps in this way the white doctors were showing insensitivity to racial realities that Black doctors know better and that are indeed medically relevant. As the organizers of the focus groups concluded, since African-Americans as a whole are far more likely than whites to suffer from hypertension and diabetes, it may be appropriate for doctors to take into account at least some population-based probabilities of disease when deciding protocols of treatment to follow. Color-blind medicine isn’t necessarily the best medicine.
The picture also looks different when researchers pan back and look at how widely medical practice varies in different areas of the United States. From this perspective, it is place, not race, that overwhelmingly determines what specific treatments patients receive for specific ailments.
Blacks tend to live in parts of the country that have a disproportionately large share of low-quality providers. But as researchers from Dartmouth Medical School have demonstrated, within poor-quality hospitals, which include not just inner-city “St. Elsewheres but often well-known academic medical centers, both whites and Blacks tend to be equally mistreated, often by being subjected to unnecessary surgery and unproven treatments. Moreover, there are some predominantly Black cities, such as Raleigh, North Carolina, and Birmingham, Ala., that have a long history of institutionalized segregation but where the researchers did not find racial disparities in treatment, and there are others, such as Jackson, Miss., where racial disparities in care are apparent.
More recently, researchers associated with the Dartmouth Atlas Project have concluded that “where patients live has a greater influence on the care they receive than the color of their skin.” Reform efforts, they argue, should therefore be focused not on the headline-grabbing issue of racial disparities, but on improving the quality of the U.S. health care delivery system in every region where it is poor.
This article originally published in the September 30, 2013 print edition of The Louisiana Weekly newspaper.



